The concept, Need and Indications for admissions to Obstetric HDU/Obstetric ICU
Introduction :
Safe Maternity is viewed as a basic human right worldwide. Health of a woman reflects health of the nation. Maternal mortality is an important indicator of maternal health. Because of various government schemes and efforts by many organizations in India, hospital delivery rate has improved a lot and reached up to 84% and MMR has reached up to 167 deaths per 100,000 live births in 2013 in India, which is still lagging behind the Millennium Development Goals (MDGs) by 2015. MMR in developed countries is < 20. Maternal mortality is ‘just the tip of the iceberg’. There is a vast base to this iceberg – which is unseen and known as maternal morbidity (near miss). Recent WHO systematic review, global prevalence of SAMM (defined as severe life-threatening obstetric complication necessitating an urgent medical intervention in order to prevent likely death of mother), varies from 0.01 to 8.23%. The case fatality ratio is 0.02–37%. Incidence of high-risk pregnancy is approximately 15% in India. At every 5 min, one woman dies from a pregnancy related complication in India. (Unicef). Prevalence of SAMM necessitating urgent medical intervention can be as high as 8.23% in India (WHO).
An interesting study was published in The May 2013 publication in the Lanceton implementation of essential obstetric health services & outcome, showed that the immediate interventions with prophylactic uterotonics and treatment with oxytocics were given in low and high resourced countries to the same magnitude in teaching institutions. The same was applied for the use of magnesium sulphate. However the maternal mortality was high in countries which have already high mortality & low in countries which have already low maternal mortality. Several explanations were given to this observation but the most likely explanation given was the lack of appropriate level of care, team work and the absence of critical care in low resource countries after the life threatening incident has happened.
Critical care in obstetrics is required becauseany pregnant woman can develop life-threatening complications with little or no advance warning. Care of critically ill patients is a unique challenge in obstetrics as deterioration is fast and there may be an existing comorbid medical condition. Pregnancy may modify the disease state. Drug therapy may be affected by altered pharmacokinetics. Drug therapy may have impact on the foetus. In UK, nearly 30% big hospitals are having High Dependency care Unit facility. In our country, the facility was nearly nil before 2010. Therefore, these women are being managed in the labour rooms or routine wards without monitoring facilities and trained health care providers. In order to provide timely care to these mothers and reduce preventable maternal deaths, close monitoring and skill-based services by trained professionals in a dedicated obstetric HDU/ICU with state-of-the-art technology is the need of the hour.
Obstetric ICU/HDU :
Obstetric ICU is an ICU dedicated to manage only for obstetric patients having critical obstetrical or medical or surgical complications, managed by staff oriented for obstetric physiology and pathology.
An Obstetric high dependency unit is an area in the obstetric department where patients can be cared for more extensively than on a normal ward, but not to the point of intensive care. So it is known as intermediate care units. Patients may be admitted to an HDU because they are at risk of requiring intensive care admission (step up) or at the same time, patients in the Intensive Care Unit who have had an improvement in their condition require a stay in the High Dependency Unit (HDU) before admission to a general ward (step down). HDU would not normally accept patients requiring mechanical ventilation, but could manage those receiving close monitoring. Patients with multi organ failure cannot be kept in HUD but patients requiring single organ support can be admitted in HDU.
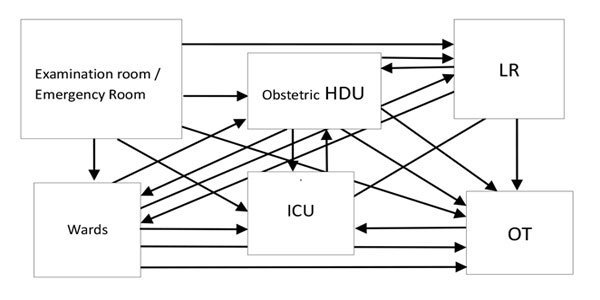
Critically ill obstetric patient is safer if admitted in Obstetric HDU/ICU than MICU because if required,patient can be shifted easily and promptly to LR or Operation theatre, neonates can be taken care better as NICU is near and Foetal monitoring is also possible.Obstetric HDU and Obstetric ICU are nearer to each other in the obstetric department and so step up and step down facility can be used easily.In Obstetric ICU, beds have the facility to be converted into labour table.In Obstetric HDU/ICU, a trained or experienced dedicated full time obstetrician and staff is trained in obstetric complications/emergencies is always available.
Triage policy : Patients may be transferred directly to Obstetric HDU/ICU from an emergency department if required, or from a ward if they rapidly deteriorate, or immediately after surgery if the surgery is very invasive and the patient is at high risk of complications.Depending on the clinical condition and severity of illness, the Obstetrician will take decision whom to admit in obstetric HDU/ICU or who will require routine care / delivery.
Admission Indications : Obstetric disorders constitute 2/3 of admissions and 1/3 is due to pregnancy with medical disorders in obstetric HDU/ICU. Antenatal admissions are more common with medical complications and hypertensive disease of pregnancy while post-partum patients are admitted more with hemodynamic instability mostly from obstetric haemorrhage, infection and post-operative complication.
During examination, a quick initial assessment is done. Obstetric Patient with following conditions/diagnosis may require admission in Obstetric HDU:
- Hemodynamic instability
- Respiratory dysfunction
- Neurologic complications
- Acute kidney injury
- Hematological complications
High Dependency care unit admissions are mainly constitutes of high risk patient likely to develop problems, having Single organ dysfunction, requiring minimal O2 support, blood transfusion or non invasive monitoring. Obstetric ICU admissions are mainly constitute of patients requiring two or more organ systems support, Invasive monitoring, Ventilatory support, Inotropic support, massive blood transfusion, renal replacement therapy, risk of sudden catastrophic deterioration or multidisciplinary team is required.
Patient with following parameters require admission in Obstetric HDU/ICU:
| Obstetric HDU | Obstetric ICU |
|---|---|
|
|
SCOPE OF HDU: Following conditions may require admission in Obstetric HDU/ICU
| Obstetric Complications | Pregnancy with Medical Complications |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Other conditions when Obstetrician decides that it is appropriate to admit her in Obstetric HDU/ ICU.
Isolation: Pregnancy with H1NI, Pyometra, HIV and infectious diseases should be admitted in Isolation Room in Obstetric HDU/ ICU.
While shifting or referring of a patient to Obstetric HDU/ICU, the decision has to be informed to relatives & consent is taken, patient should be escorted by doctor /staff with case sheets and all existing treatment including oxygen and patent IV line, monitoring the vitals of the patient should be continued and ensuring patent airway. Baby should be shifted with mother if she has delivered.
A Study was conducted at Santokba Durlabhji Memorial Hospital, Jaipur to analyze the role of HDU/SDU in obstetric critical care settings. Women admitted in HDU/ICU over 3 years (2009-2012) were studied. Out of 594 high risk women, 427(72%) were managed in HDU and 167(28%) required ICU. Out of 167 women in ICU, 109(65%) were shifted from HDU and 58(35%) were admitted directly. Out of 427 women in HDU, 400(93.6%) discharged in good condition, none expired and 27(6%) were LAMA. Out of 167 in ICU, 106 discharged in good condition, 35(21%) expired and 26(15.6%) were LAMA. In their study, it was found that burden of ICU was reduced to 1/3rd compare to last 5 years and expenditure of hospital in maintenance of ICU decreased by 41%. Total treatment cost to the patient decreased by 38%.
A retrospective observational study was carried out from May 2007 to May 2011 in the Dept. of Obstetrics and Gynecology and HDU of IPGME and R, Kolkata. In their study, Obstetric HDU utilization rate was 11.2 per 1000 deliveries. Out of total 57 subjects 48 had no prior antenatal care. Majority (68.42%) admitted in HDU with only obstetric reasons, while 31.57% required HDU for pre-existing medical diseases. The major obstetric indications were septicemia (35.08%), PPH (29.08%) and hypertension was observed in 21.05% of women. Other less common causes included post surgical acute kidney injury, APH, chrioamnionitis and pyelonephritis. Half of the women with pre-existing medical disease had cardiovascular problems. Patients with medical diseases had more pre-term labour (10 vs 5; P ≤ 0.05), respiratory failure (9 vs 2; P ≤ 0.05), cardiac failure (7 vs 1; P ≤ 0.05), duration of stay more than 10 days (15 vs 6; P ≤ 0.05), foetal growth restriction (6vs 3; P ≤ 0.05) and prolonged recovery time. Maternal mortality was 12.28% and foetal mortality was 17.54%.
Another study was done to establish the utilisation of high dependency care in a tertiary referral obstetric unit.Data of pregnant or recently pregnant women admitted to the obstetric HDU from 1984 to 2007 were included to evaluate the admission rate. Four years' information of an ongoing prospective audit was collated to identify the indications for admission, maternal monitoring, transfers to intensive care unit, and location of the baby. The overall HDU admission rate was 2.87%, but increased to 5.01% in the most recent 4 years. It was found that massive obstetric haemorrhage is now the most common reason for admission. Invasive monitoring was undertaken in 30% of women. Two-thirds of neonates (66.3%) stayed with their critically ill mothers in the HDU. Transfer to the ICU was needed in 1.4 per 1000 deliveries conducted.
In Rotunda Hospital, Dublin (Ireland), a study was conducted to assess HDU utilisation rate, to determine the indications for and rate of transfer to an intensive care unit (ICU) in a tertiary referral centre. A 4-year retrospective review of case notes and HDU/ICU registers was performed. One hundred and twenty-three patients were admitted to the HDU in the 2 years following its inception, representing 1.02% of all deliveries. Obstetric complications accounted for 81.3% of admissions. The incidence of HDU utilization reveals just the tip of the iceberg. 17 patients were transferred to a general ICU, 12 before the HDU was established (representing 0.08% of all deliveries) and 5 after (0.04%). Although not statistically significant, there is an apparent trend toward decreased ICU admission rates following the establishment of the HDU. Length of stay in ICU was 3 days before the HDU was established and 2.0 days after HDU. Before HDU, transfer to ICU was predominantly because of haemodynamic instability. Following the advent of the HDU, the need for mechanical ventilation became the major indication for maternal ICU admission as good number of patients with haemodynamic instability being managed within the HDU. There was no maternal mortality.
Wheatley et al. suggested that early intervention and treatment of the critically ill obstetric patient might prevent serious complications and avoid the need for ICU. In their study, almost 60% of the patients admitted to ICU could have been managed appropriately within the HDU setting.
The proportion of obstetric patients requiring admission to intensive care units (ICUs) varies among published series at between 1 and 9 per 1000 deliveries, with obstetric complications accounting for the majority of admission diagnoses. Bouvier-Colle and colleagues estimated a rate of 3.1% and Mabie & Sibai found a rate of 0.88%.
It is important to provide critical care services to obstetric patients as they are young, otherwise healthy. Every year 3.03.000 pregnant women die in the world (WHO-2015). It is said that, if quality obstetric health care is provided in time, then we should save 80% of these women in the world. Dedicated obstetric HDU/ICU means an establishment, a facility, quality care and the need of the hour.
For further reading:
- WHO multicountry survey on maternal and newborn health The Lancet. 2013:381(98791747–1755.
- Journal Anaesthesia, 2008, 63, pages 1081–1086 by K. Saravanakumar, L. Davies,M. Lewis, G. M. Cooper
- International Journal on critical Illness and Injury Sci. 2013 Jan-Mar; 3(1): 31–35.
- https://www.ncbi.nlm.nih.gov/pubmed/11121922, by Ryan M, Hamilton V, Bowen M, McKenna P