Planning Antenatal Classes
Guidance for conducting ANC classes

Location:
- Waiting room
- Any available room where a couple can sit together and practice certain exercises

Instructors:
- Supervision of Gynecologist is mandatory
- Midwife/Nurses should be available as attendant
- Nutritionist, Dieticians, physiotherapist may attend and take sessions on Nutrition & exercise respectively
Time

Morning session

Afternoon session

Evening session (Working moms)
Planning Antenatal Classes
Content for ANC classes

Contents:
- Preconception care
- Understanding your pregnancy
- First trimester
- What to expect?
- How to prepare?
- Danger Signs
- Second trimester
- Third trimester
- Labor & delivery
- Meeting your baby and the first few hours after birth
- General Advice
- Foods
- Exercise
- Dos & Don'ts
- Treatment of common ailments
- Q & A
- Postnatal care
- Breastfeeding
- Infant care
- Tips for the dads
Preparing for motherhood
Antenatal care program Duration of presentation – 4 hours
Plan your pregnancy !
Because the best time is before...

Preconception Care
First Trimester
Second Trimester
Third Trimester
Enhancing Your Experience of the Journey towards Motherhood ...
We will guide you every step of the way!
Preconception Care
Prepregnancy care : To bring out the best in you!

Balanced diet and exercise

Correct supplements (Folic acid 400ug/day)

Avoid alcohol/smoking

Is weight a problem? (Overweight/underweight)

Are you on any medications (diabetes, epilepsy)? Review plan with your doctor

Take basic tests: Hb/BG/Blood sugar/TSH/Rubella IgG/HIV

Ask your doctor about vaccination if required; Rubella/Varicella/Tdap/HBV
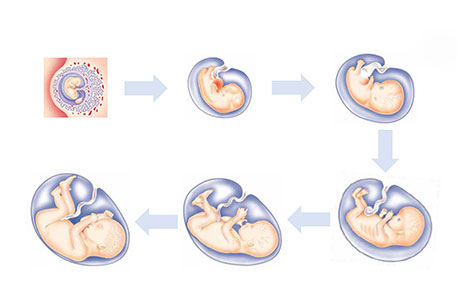
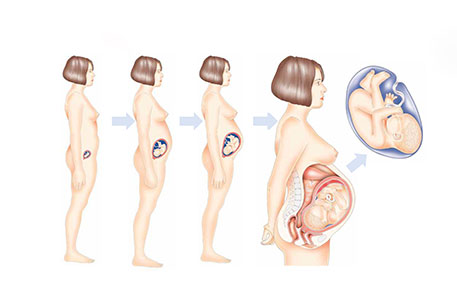
Understanding Pregnancy Changes
Knowing What goes on Inside till it comes out!!!
First Trimester (0-13 weeks)

What to expect?
- Urine pregnancy test can be positive on the first day of your missed period
- You may experience cravings, morning sickness, fatigue, frequent urination

How to prepare-1?
The tests
- Seek an appointment with your doctor to confirm a normal pregnancy after a urine pregnancy test is positive
- Discuss various tests that need to be done at this stage
- Hb/BG/HIV/HBSAg/VDRL/Blood sugar/TSH/Urine examination
- First USG for confirming a live baby
- Next USG at 11-14 weeks (for any abnormality in the baby)
- Double marker test to rule out abnormality
How to prepare-2 ?

Balanced diet

Avoid smoking/alcohol

Folic acid (400 micro grams/day)

Regular exercise

Decide where you want to get booked and deliver

At least once a month visit to your doctor
Do you have any special Concerns ?
Inform your doctor if you have:
Any long standing illness (diabetes, hypertension, seizures etc)
Any past infection (HIV, HBV, TB)
Any history of taking medication for any ailment or previous surgery
Tell us to care for you better!!!
Danger Signs
Report immediately if there is :
- Bleeding from the vagina
- Excessive discharge from the vagina
- Excessive lower abdominal pain or abdominal cramps
- Dizziness
- Excessive vomiting
- Fever with or without a rash

Second Trimester 14-26 weeks
- Troublesome symptoms of first trimester fading
-
14th week:
- Baby‘s heartbeat becomes strong and can be heard using an ultrasound detector
- Stretch marks start appearing on abdomen
-
16-18 weeks:
- Baby’s movement can be felt
-
26th week:
- Baby’s eyes and ears begin functioning, baby can open and clench hands
- Your pregnancy may just be beginning to show. This varies a lot from woman to woman
The tests
- Ultrasound at 18-20 weeks to look for anomalies in the baby
-
Blood tests:
- Triple or quadruple test(16-18wks ) if the first trimester screening is incomplete (11-14 wks scan +Double Marker)
- GTT with 75 gms glucose to rule out diabetes
- Additional tests according to any high risk condition e.g. ICT if Rh Negative
- Your doctor will check your BP and urine at each antenatal visit
- Your doctor will check the height of your uterus
- You should be taking your iron and calcium supplements
- It is time for your tetanus shot (two/one depending on your previous history of vaccination)
- Antenatal Visits every 3-4 weeks.
Report immediately if there is :
- Bleeding from the vagina
- Excessive watery discharge from the vagina
- Excessive lower abdominal pain or abdominal cramps
-
Symptoms of High BP
- Headache
- Epigastric Pain
- Blurring of visio
- Swelling over the body
- Increased frequency of urination(UTI)
- Excessive fatigue (anemia)
The final Countdown: Third Trimester (27-40 weeks)
- Baby is now completely formed
- There is increased fatigue
- There might a tightening of uterus from time to time without actual pains(Braxton Hicks Contractions)
- Sleeping becomes difficult
- There is a little relief after 36 weeks when the baby goes down into pelvis and you can breathe easy (Lightening)
The tests
- Good idea to repeat a hemoglobin at this stage (32 weeks) to see if any correction needed
- Ultrasound needed if there is doubt about the growth of the baby
- A routine USG to look for the growth and weight of baby at 32-34 weeks may be offered by some
- Your antenatal visits would be more frequent (every 2 weeks after 34 weeks )
- Your doctor would measure BP and urine for proteins at each visit
- You would be examined for anemia or any swelling in the feet
- Your doctor would measure the size of the uterus with or without a tape
- If you are Rh negative and your ICT has been negative , now is the time to take Anti D Injections
- You continue taking iron and calcium supplements
- Wear comfortable shoes. Try resting with feet up to avoid swelling
- Discuss plans for labor and deliver:
- Route of delivery
- Place of delivery
- Delivery companion
- Gather information on:
- Feeding / caring for the baby
- Newborn tests
- Baby blues/ post partum depression
- What if I don’t go into labor?
- Till when should I wait for labor to happen?
- Can my pregnancy be electively terminated; When would that happen (Induction)?
- What are my chances of having a normal versus a caesarean deliver?
- Intermittent pain starting from back coming to the front of the lower abdomen with tightening of the uterus
- Bleeding from the vagina
- Rupture of the bag of membranes with sudden gush of watery fluid
- Thick sticky discharge from vagina
- Decreased perception of fetal movement
Labour & delivery
Preparing for birth
As your third trimester starts, your attention starts shifting from pregnancy care to how your delivery will take place. There is a lot you can do to prepare yourself for birth.
GENTLE EXERCISE
Build up your stamina. Make sure you continue a gentle form of exercise, such as walking every day for at least half an hour. If the weather is hot, choose a time of the day when the sun is not shining strong, such as early morning or at dusk. Make sure you always carry water with you and sit as often as you feel like.
PERINEAL MASSAGE
Massaging the vagina and perineal area in the last weeks of pregnancy, (from about 34 weeks onwards) has shown to help the vagina stretch during birth. This might reduce the need for an episiotomy.
PACKING YOUR HOSPITAL BAG
By the time you are about 36 weeks pregnant, you should pack your hospital bag. Once you are full term, at 37 weeks, your baby can be born at any time. In your hospital bag, you'll need a few items for the days you will spend in the hospital and a few essentials for your newborn's first days.
What to pack for the delivery
- Copies of your medical records
- Slippers
- The hospital might have a gown they want you to wear instead of your home clothes once you get admitted
- An old nightdress or a comfortable sleep shirt/Tshirt to wear during labour
- Massage oil or lotion if you would like to be massaged during your labour
- Lip balm
- Pictures of someone or something you love. They could be the inspiration you need to see through to the end
- An elastic band or hair clip. You might want your hair tied up or pulled back during labour
- Things to help you relax or pass the time, such as music, books, magazines
What to pack for after the birth
- A stole or dupatta to cover yourself while breastfeeding
- Breast pads to soak up any leaking milk
- A going-home outfit. It will take a while for your tummy to go down, so you'll still need your maternity clothes for the first few weeks after birth.
- Front-opening ones (feeding gowns) are useful for breastfeeding
- Panties. Don't bring your best ones as they will get messy. Choose ones with a high elastic band so that if you end up having a caesarean, the band doesn’t lie on or near your wound
- Toiletries (hairbrush, soap, shampoo, deodorant, tooth brush, tooth paste and face wash, towel)
- Any medication you are on
- Maternity/sanitary pads
What to pack for your baby
- A couple of baby outfits that are suited to the season (cotton jhablas, rompers sleep suits, T-shirts, shorts or leggings, will all work well
- Muslin or soft cotton cloths to clean up vomit or spills during breastfeeding sessions
- Blankets, socks, booties, caps
- Innerwear such as onesies or vests. Jumpers for winter babies.
- Nappies - your baby will pass urine at least 12 times in 24 hours and may pass bowel movements several times a day
- Baby wipes, Toiletries (baby soap, shampoo, hairbrush, nail clippers, towel)
- Waterproof sheet protector or rubber under sheet to keep the bed from getting wet with spit-up, pee or breastmilk
- Soft cotton sheets for your baby to sleep on, A changing mat
Signs of labour
- About a month before your due date, or if this is your second baby, closer to your delivery, your baby's head moves down into the pelvis in preparation of birth. This is known as engagement or lightening.
- You may feel like you suddenly have more space for your lungs and stomach, but you may also feel your baby's head very low down. This can put a lot of pressure on your bladder, so you might be making more frequent trips to the loo.
- As you approach your due date, you might start getting contractions. These are practice contractions that can be painful, or they may just feel like your whole tummy is turning into a hard ball for a few seconds at a time.
Other signs that labour has started or soon will
A show is a vaginal discharge of mucous, often tinged with blood. This is the mucus plug that has kept your cervix closed for the past nine months. Labour contractions can start soon after a show, or they may not happen for another week or so.
If you get a slow trickle or a gush of fluid from your vagina, it is usually a sign that your water has broken. If your water has broken, go to the hospital, even if labour contractions have not started yet. If you suspect you are in labour but are not sure what to do, call your doctor. She will tell you when you need to come to the hospital. Most doctors will ask you to come and get checked. If it is a false alarm, you will be sent home. If you really are in labour, you'll be admitted. Especially if this is your first baby, labour can take a long time. So go to the hospital with a few things from home that will help to keep you distracted and take your mind off the contractions.
Checks and procedures on arrival at the hospital
- Once you reach the hospital for your delivery, your doctor will check you. If you are in labour, she will want to know how far your labour has advanced. She will judge this by how far apart your contractions are, and how much your cervix has dilated. She will also feel your stomach for the position of your baby.
- Most babies are in a head down position by the time you reach full term, but some babies stay head up and bottom down – a position known as breech. If you have a breech baby, or if your baby is laying sideways, also known as a transverse position, your doctor will suggest a caesarean delivery.
- Once your doctor has done a standard check, in most hospitals, the nurses will do an enema. An enema is a procedure by which the contents of your large intestine are washed out. It can be quite uncomfortable because a catheter is inserted into your anus. An enema is done, so that you do not pass stool as your baby comes out.
- The nurses will then shave your private parts. If you are going in for a caesarean, they will shave from your belly button down. If it looks like your labour may take a while, your doctor might suggest that you walk around the room. Walking and moving around can help to shorten labour.
- Make sure you walk with someone, so that you have support when a contraction starts. If you cannot walk around, ensure that you sit as upright as possible in your bed. Or you can kneel on the floor and lean forward onto a chair or sofa in the room. Being upright means that gravity helps your baby move down with each contraction.
- Your doctor might also offer you a drip to speed up labour. The drip will contain Syntocinon, which is an artificial form of oxytocin, the labour hormone. Oxytocin shapes the frequency, length and strength of your contractions. Giving you an added dose of the hormone helps to speed things along. If you have Syntocinon, your baby's heartbeat will be continuously monitored. Your doctor will strap electronic sensors to your tummy to keep a track of her heartbeat.
The stages of labour
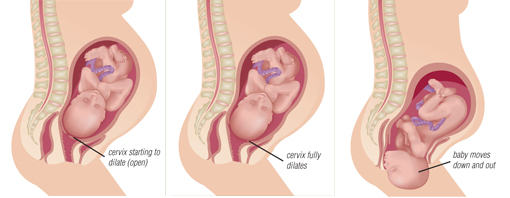
A vaginal or normal delivery happens in three stages
CONTRACTIONS OPEN UP THE CERVIX
The first stage of labour is the time that your contractions open the cervix. This happens in three phases:
- Early labour
- Active labour
- Transitional phase
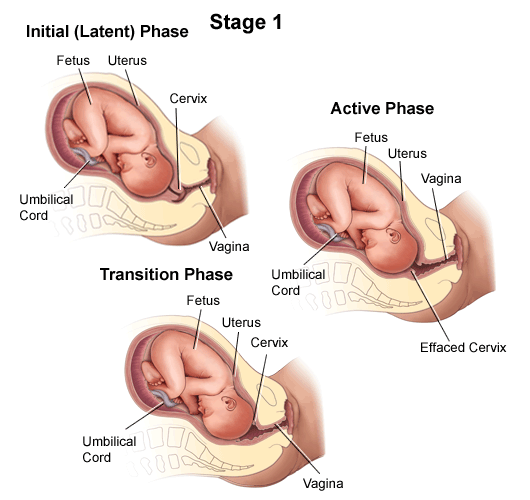
- The early phase is sometimes called the latent period or prelabour.
- The womb starts to contract or tighten regularly. The contractions start off being bearable but gradually become more frequent and painful.
- As the cervix begins to open, it gets thinner and softer. This phase can last a few hours or span out over a few days.
- Early labour is best spent at home if you have had an uncomplicated pregnancy, so that you can be comfortable and relax as much as possible. But some doctors prefer to monitor you right from the start. So call your doctor to be sure about how long she recommends you stay at home and when to come to the hospital.
- When your cervix has dilated to 4cm, active labour starts.
- Your contractions will get stronger and more frequent. They will also last longer. Eventually they may be coming as frequently as every three to four minutes and lasting 60 to 90 seconds.
- This phase of labour can last between 5 to 18 hours and is usually best spent in hospital. This is the time that many mums ask for pain relief.
- During the transitional phase, the cervix dilates from 8cm to 10cm. Contractions may last for over a minute and come every two to three minutes. You might feel shaky, shivery and sick.
- This is often the most painful and intense part of labour and can last between a few minutes to an hour.
YOUR BODY PUSHES YOUR BABY OUT
- When the second stage of labour begins, you will feel the urge to push. This usually happens when your cervix has fully dilated to 10cm. If you are not yet fully dilated, your doctor might ask you not to push. But the urge is so strong it can be hard to ignore.
- There are some breathing techniques and labour positions that help you not to push. For example, getting on your hands and knees or panting can help. Your doctor will tell you when to pant and when to push. Just before your baby comes out, your doctor will probably cut the back of the perineum (wall between the vagina and anus). This cut is known as an episiotomy.
- Doctors usually perform an episiotomy to make more room for your baby to be born. Your doctor should ideally offer you an episiotomy only if she feels that you will benefit from having the procedure. For example, you may need an episiotomy if your baby is distressed and needs to be born quickly, or you've been pushing a long time. If you have an episiotomy, the cut will be stitched up after the birth
DELIVERING THE PLACENTA
- The third stage of labour begins once your baby is born, and ends when you deliver the placenta.
- The placenta gets detached from the wall of your womb as it starts contracting down after the birth. Your placenta can be delivered naturally, or you can have what is known as a managed third stage of labour.
- If you have a managed third stage, your doctor will give you an injection in your thigh as soon as your baby's shoulder emerges. The injection stimulates strong contractions in your womb. This makes your placenta peel away.
- Once the birth is over, you may feel shaky due to the adrenaline in your system and the adjustments your body immediately starts to make, or you may be very emotional, exhausted or euphoric! Some women find it hard to pay attention to their baby if they have had a long labour, or if they've had painkilling drugs such as pethidine.
- If you feel exhausted, take your time. After a rest, you will be much more interested in getting to know your baby.
PAIN RELIEF IN LABOUR
- Nobody knows exactly how labour will feel for them until it starts. While you may decide against using any pain relief, you might happily agree to some once the time comes. Or you might be set on having an epidural and then find that you have to manage without it. The important thing to remember is that there's no right and wrong when it comes to pain relief.
- You don't need to decide now what you will use during labour, if anything, but it is a good idea to be well informed about your options. This way, you will know what pain relief to ask for if you feel the need for it, and you will understand how each pain relief method works and the effects it has on your baby.
THE DIFFERENT METHODS OF PAIN RELIEF THAT ARE AVAILABLE
There are several things you can do to help with labour pain. Natural pain relief methods such as:
- Massage
- Breathing techniques
- Changing positions
- Resting
might help to numb the pain and reduce the need for drugs.
- TENS stands for transcutaneous electrical nerve stimulation. A TENS machine has pads that you stick on your back.
- The pads give out little pulses of electrical energy which help to ease some pain.
- A TENS machine takes the edge off a contraction rather than numbing the pain completely.
- Gas and air (also called Entonox) is a colorless and odorless gas that has a calming effect. It makes labour pain more bearable, rather than blocking the pain completely.
- It takes at least 30 seconds for it to take effect, so you need to start breathing the gas and air the very second you feel a contraction beginning.
- If you wait until the contraction really hurts, and then start breathing, it will not be effective.
- An epidural is a type of regional anaesthetic. It is a very effective form of pain relief and can be given at any point during labour.
- It is given by inserting a fine tube into the spinal column at the small of your back. Having an epidural makes labour and birth a much more pleasant experience for many mums, but it can also make other interventions, such as speeding up labour or using forceps or ventouse to help your baby out, more likely.
- A spinal is an anaesthetic injection into the spine that acts faster than an epidural. Unlike an epidural, no tube is left in the spine.
- It is used to top up an epidural or given if an emergency caesarean or other procedure is required.
- Pethidine is a painkilling drug and it also helps you relax. It is not used very often because it can pass through the placenta to your baby. If used, it is given during the first stage of labour, well before you start pushing.
- Using it when you're close to giving birth can make your baby too sleepy to breathe and feed properly after birth. Your doctor or a nurse will check how dilated your cervix is before giving you this drug.
A caesarean (or 'c-section') is an operation in which an obstetrician makes a cut through your belly and womb so that your baby can be born. It's the most common major surgery that women have.
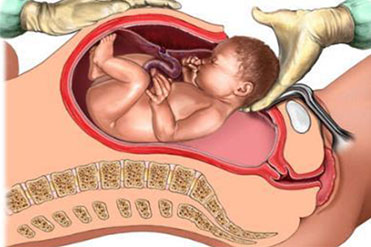
COMMON REASONS FOR HAVING A CAESAREAN
Your baby is in a breech (bottom first) or transverse (sideways) position.
Your baby has a known foetal illness or abnormality that requires a caesarean birth.
Diabetes or gestational diabetes has caused your baby to grow too big for a normal delivery.
You have placenta previa (when the placenta is implanted so low in your uterus that it blocks your baby's exit).
Your pre-eclampsia is rapidly worsening, making it dangerous to delay delivery.
You have a history of uterine surgery or multiple caesarean sections.
- These conditions can be diagnosed well before your due date and so your doctor will tell you to expect a caesarean delivery. Sometimes, complications during labour and birth mean that an emergency caesarean is necessary. This can be hard for the mother since often it means a few hours of labour before getting a caesarean.
- Even if none of these conditions apply to you, your doctor may schedule an elective caesarean if you wish to give birth this way. This would typically happen if you do not want a vaginal birth for a specific reason.
- Occasionally, a doctor may perform an elective caesarean if a woman and her family want the baby to arrive on a particular auspicious day, for astrological reasons. But this is generally not recommended because a caesarean is a major operation. It can really help you to cope with a caesarean if you take time now to think about what might happen during and after the operation.

WHAT HAPPENS DURING A CAESAREAN
- You will be made to remove all your jewellery, make-up and nail polish. This is so that your skin tone can be monitored during the operation. You won't be able to wear contact lenses or glasses either.
- A sample of your blood might be taken to check that your iron levels are high enough and you haven't got anaemia. If you are anaemic and happen to have huge blood loss, you will need a blood transfusion.
- You'll be given an anaesthetic. Usually, regional anaesthesia such as a spinal or an epidural is used. This type of anaesthesia numbs your bottom half and is safer for you and your baby than a general anaesthetic, which puts you to sleep.
- A drip will be inserted into a vein in your arm. This will give you fluids and make it easy to give you drugs if you need them during the operation or later.
- A thin tube, or catheter, will be inserted into your bladder via your urethra. This will make sure your bladder is empty. The catheter will stay in place after the operation until you regain sensation and can control your bladder independently again.
- The area on your tummy where the cut will be made will be shaved and cleaned with an antiseptic. Then it is covered with special sterile sheets, which are cut in the centre, so that only the part to be operated on remains exposed.
- Your blood pressure will be taken and your heart rate will be monitored at all times.
- You'll also be given an injection of antibiotics to ward off infection and anti-sickness medicine to stop you from vomiting, which is a common side-effect of the anaesthetics.
- Once you are ready for the operation, the doctor will make a small horizontal cut into your skin - about two fingers' width above your pubic bone. This type of cut is called a bikini cut.
- Your doctor will then open the layers of tissue and muscle to reach your uterus. When your doctor opens up your uterus, she then breaks the sac your baby is in. You may hear fluid gushing out. Your baby is then lifted out. You may be aware of the assistant pressing on your belly to help your baby be born. It only takes a few minutes from the time the doctor starts the operation until your baby is born.
- Your baby will be quickly checked over by the pediatrician. He will then be brought to you.
- After your baby is born, your doctor will gently tug the umbilical cord to pull out the placenta. She will then concentrate on stitching you up. Each layer of muscle and skin needs to be closed using clamps, staples, or sutures.
- When you're ready, you'll be moved to your room where you, your husband and your baby can be together. If there is a need for it, your baby might be moved to the neonatal intensive care unit (NICU) instead where he will receive specialized medical care.
- You may start shivering, because your body temperature drops during the operation. Your nurse will warm you up with blankets and help you breastfeed your baby. You may find it more comfortable to breastfeed if you both lie on your side and face each other. It often takes some time to find a comfortable feeding position after a caesarean, but it's worth persevering for both you and your baby’s sake, and it does get easier.
MEETING your baby AND THE FIRST FEW HOURS AFTER BIRTH
SKIN TO SKIN
- The first few hours after birth are important. Your baby goes from a warm and protected environment to a whole new world of lights, sounds and sensations.
- As your baby adjusts to this new world, she may calmly take it all in or respond the only way she knows how, by crying lustily.
- You can help her by soothing her with the sound of your voice and holding her, skin-toskin.
- She will recognize your voice, the sound of your heartbeat and your smell.
APGAR SCORES
At one minute and again at five minutes after birth, your baby will be checked and given a score from zero to two for five factors that will measure her wellbeing. This is known as the Apgar scale and it looks at your baby's:
- Appearance (skin tone)
- Pulse rate (heart rate)
- Grimace (reflex response)
- Activity (muscle tone)
- Respiration (breathing)
The scores are added to reach a maximum of 10 points. Most newborns score between seven and 10, which mean they do not need any treatment. A difficult or premature birth, or pain relief such as pethidine during labour, for example, can affect your baby's wellbeing after birth and lower the scores.
VITAMIN K
- Soon after birth, your baby will get an injection of vitamin K, as a preventative measure against a rare complication called vitamin K deficiency bleeding.
- This is because vitamin K is needed for blood clotting, and babies are born with small amounts of vitamin K.

FIRST VACCINES
- Before you leave the hospital for home, your baby will also get her first vaccines against some serious illnesses: BCG, which protects against tuberculosis, Hepatitis B vaccine (Hep B) and polio drops (also called oral polio vaccine or OPV).
FIRST FEED AND THE FIRST FEW HOURS AFTER BIRTH
- Ideally, your baby should get her first feed of breastmilk within the first hour of birth, but this may not be possible if you've had a difficult birth, or your baby needs special care.
- If your baby is placed on your chest, skin to skin, she may wriggle to your breast and feed, or she may only smell, lick or nuzzle your breast. All these things will help you and your baby get breastfeeding off to a great start.
- The first milk your body produces is known as colostrum. It is thicker and often more yellow in colour than regular breastmilk.
- This first milk is extremely good for your baby. It is with antibodies that will help your baby fight infections and viruses in the coming days. It is also rich in protein and it has a laxative effect that helps your baby pass her first bowel movement.
- For the first hour, your baby will probably be quite alert, but she'll soon need a long sleep to recover from the physical strain of birth. This is a good time for you to catch up on some sleep as well. If you feel bruised and battered, tired or disappointed, don't be hard on yourself. It doesn't mean you won't love your baby, or you won't be a wonderful mum. You're just exhausted and in need of a good rest. You'll have plenty of time in the days and weeks to come to build a strong and loving relationship with your baby
- Advantages of Breastfeeding

Recovering FROM BIRTH
Staying in hospital
- How long you stay at the hospital will depend on the kind of delivery you have had. You will need to stay longer if you have had a caesarean, but can usually go home on your third day if you had a normal delivery.
- Once you get home, you will have your precious baby to look after, but you will also need to take care that you recover well from the huge physical upheaval that is giving birth.
Lochia
- One of the first things you will notice after your delivery is that you have bloody discharge. This bleeding, known as lochia, happens whether you've had a vaginal birth or a caesarean section. It is how your body gets rid of the lining of your womb.
- The bleeding may come out in gushes or flow more evenly like a normal period. You may bleed for as little as two to three weeks or as long as six weeks after birth. Make sure you have a good supply of thick maternity pads.
Postnatal urinary incontinence
- Many women also have trouble controlling their bladder for a while after giving birth. You might find that when you cough, laugh or sneeze, some urine leaks.
- Postnatal urinary incontinence is very common. In most cases, it is a temporary problem that you can resolve within a few weeks or months with a little effort. Do regular pelvic floor exercises. They are the best way to help the problem. To see real results, you need to do them regularly, several times a day, for at least three months.
- An added bonus is that these exercises increase blood flow to your perineum, which helps stitches and bruising to heal faster.
Stitches
- Most women come home after their delivery with stitches, whether from a normal birth or a caesarean. It is important to keep the area of your stitches clean, so that no infection settles in.
Foods
Eat a variety of food to get all the nutrients

Extra 300 Calories

3-4 glasses of milk

Dairy products: 4 servings

Fruits : 2-4 servings

Bread & grains:6-11 servings

Protein products : 3 servings

At least 6-8 glasses of liquids

Sweets, spices, fried in moderate quantity only

High fibre diet: Whole grain breads, cereals, pasta, rice, fruits, vegetables

Dairy products: 1000-1300mg calcium in daily diet

Vitamin C everyday: Oranges, grapefruits, strawberries, papaya, boroccoli, tomatoes

Source of folic acid: Dark green leafy vegetables, legumes, beans, chickpeas, black beans

source of Vitamin A: Carrots, pumpkins, sweet potatoes, spinach, apricots
Foods: Keep Iron Level Up
- Take iron supplements prescribed by your doctor
- Iron pills not to be taken on empty stomach
- Don’t drink milk with iron rich meal
- Don’t take tea, coffee with meal or iron supplement
- Cooking in iron vessels may increase iron content of food. Do this no more than 2-3 times a week
- Add few drops of lime to dal,curries, sprouts or other iron rich food
- You can also drink lemonade or orange juice with your meals
- Sources of iron: green leafy vegetables, cauliflower, fenugreek, mint, lentils, beans, chicken, fish, egg, dried fruits such as apricots, raisins

Food: To Avoid
- Avoid raw and uncooked food
- Unpasteurized milk or cheese
- Fish high in mercury content
- Excessive intake of caffeine
- Alcohol intake
- Artificial sweeteners
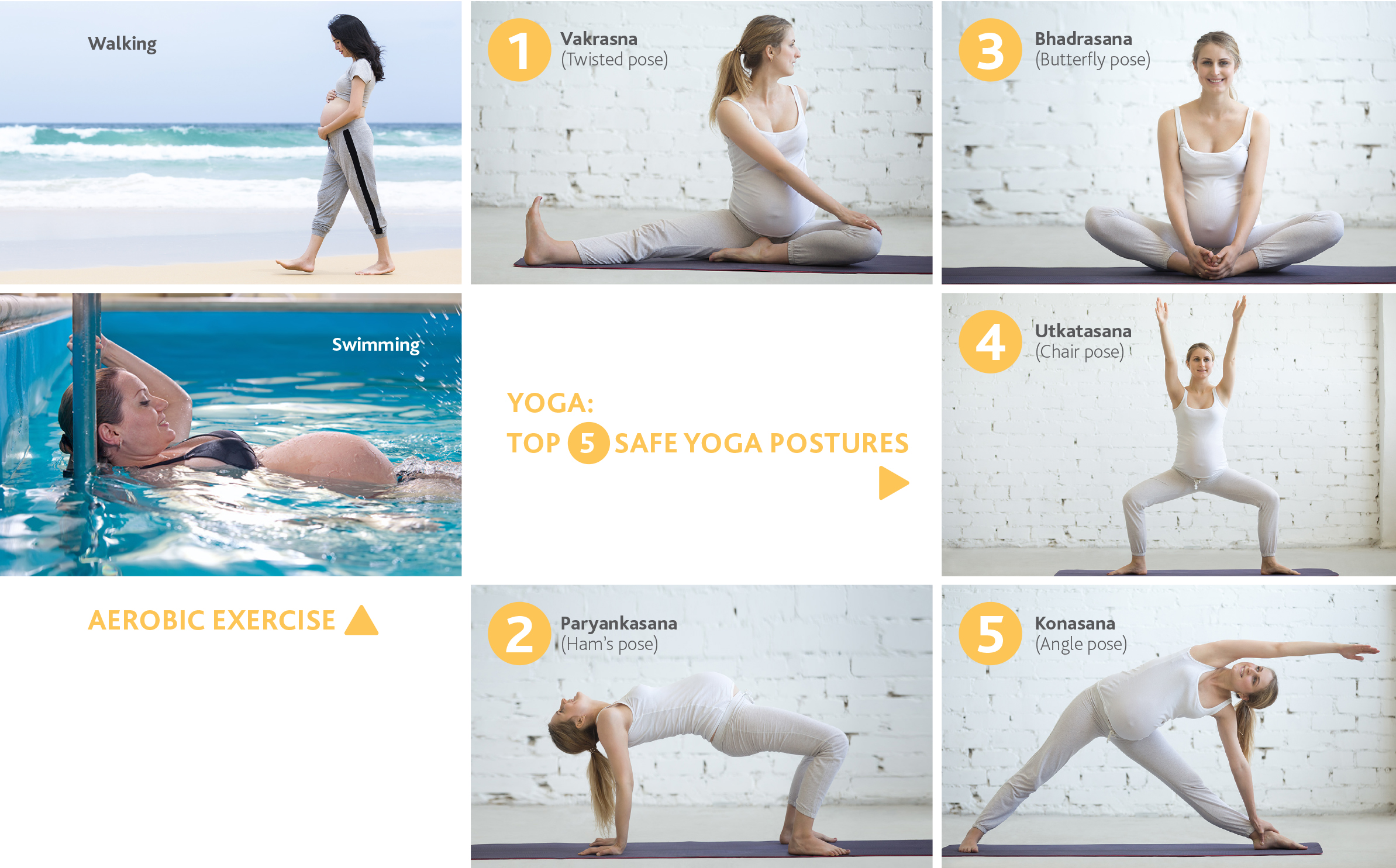
Exercise
- Exercise improves muscle tone, prevents low back pain, decrease chances of varicose veins, leg cramping, reduces constipation, improves mood
- Exercises which can be done: walking, swimming, cycling on stationary bike
- Aim for at least 30 min of daily moderate intensity activity
- Avoid lifting very heavy weights
- Do not overexert yourself or exercise upto exhaustion
- Eat a light snack 30-60min prior to workout, drink water
- Do not exercise if you have hypertension, ruptured membranes, bleeding per vaginum, preterm labour, incompetent cervix, other medical conditions
- Stop exercise if shortness of breath, vaginal bleeding or loss of fluid from vagina, uterine contractions, chest, leg, joint or stomach pain

Yoga: Top 8 safe Yoga postures

Month 1: Poorna Titali Asana (Full Butterfly Pose)

Month 2: Kashta Takhshan Asana (Chopping Wood Pose)

Month 3: Utthanasana(Squat and Rise Pose)

Month 4: Vajrasana (Thunderbolt Pose)

Month 5: Meru Akarshanasana (Spinal Bending Pose)

Month 6: Trikonasana (Triangle Pose)

Month 8: Malasana (Garland Pose)

Month 9: Balasana (Child’s Pose)
Pelvic Floor exercises
- Imagine trying to stop passing wind and hold your flow of urine at the same time. The feeling is of squeeze and lift pulling up and in around your front and back passages
- Hold the squeeze for upto 10 seconds
- Do 3 or 4 sets, three times a day

Watch Your Posture
Standing
- While standing, do not exaggerate hollow of your back.
- Stand with feet's apart, hold your head up

Sitting
- While sitting, sit so that the whole length of your thighs supported by the seat
- if needed a cushion can be placed between the back rest and your back.
- Take support of the back of chair and sit straight

Lifting
- While lifting and carrying, do not bend your waist. Keep your back straight and bend your knees and hips

Sleep
- The best sleep position during pregnancy is sleep on side. Even better is to sleep on your left side

Getting up from a lying down position
- Always turn on your side first and get up with the support of hand
Do's & Dont's
DO’S IN PREGNANCY
- Regular monthly check up is necessary
- Eat balanced diet
- Take small frequent meals if required
- Have plenty of water
- Always remain in good, cheerful and relaxed mood and also maintain pleasant atmosphere with good ventilation and airy rooms
- A minimum of half an hour walk at fairly brisk pace is a good exercise
- Sleep at least 8 hours in night & 1-2 hours in day time.
- While picking up things from the floor, sit down & then lift
- Wear your seat belt while driving
DONT’S IN PREGNANCY
- Don’t take any medicine without doctors advice
- Don’ overeat; avoid junk food, fried or oily food
- Don’t smoke
- Don’t wear high heeled shoes
- Don’t take too much rest & avoid oversleeping
- Don’t bend down with straight legs
- Do not drive
- Don’t carry heavy weight
- Don’t wake up suddenly with a jerk
- Avoid long distance travelling
Handling Common Ailments
1. Morning sickness:
- Drink plenty of fluids
- Sip ginger candy, grate it fresh in tea or try ginger candy
- Eat small frequent meals
- Opt for cold dishes, which gives off fewer aromas
- Non greasy meals with little odor such as fresh fruits, raw almonds, whole grain toast before getting out of bed.
- Limited caffeinated foods and beverages

2. Fatigue:
- Eat foods rich in iron and protein
- Take day time naps when you can
- Regular exercise
- Take rest

2. Painful breasts :
- Eat foods rich in iron and protein
- Take day time naps when you can
- Regular exercise
- Take rest


4. Constipation
- Eat more fresh fruit and vegetables
- Drink 8-10 glasses of water a day
- Eat foods with lots of fibre
- Exercise regularly

5. Heartburn :
- Eat small, frequent meals
- Avoid spicy or greasy foods
- Try drinking milk before eating
- Don’t lie down right after eating
- Elevate the head of bed 6-8 inches when lying down
- Don’t overeat
- Avoid alcohol, chocolate, coffee and tea
6. Swollen feet :
- Rest with your legs up
- Lie on your left side while sleeping
- Take breaks from sitting or standing and take a short walk
- Exercise

7. Urinating more :
- Need to empty bladder often as growing baby puts pressure on bladder
- Can’t be helped and is normal


8.Leg cramps :
- Gently stretch the calf of your leg by pointing your toes upward, toward your knee

9. Diarrhoea :
- Eat bananas, white rice, oatmeal and refined white bread
FOR MOTHERS –TO-BE

My groin hurts !
As your womb grows larger, ligaments stretch and you feel this in your groin area. By sleeping on your side with the leg that hurts on the bottom, the ligaments will relax and pain decreases. Take enough calcium.
My skin is becoming dry!
As your pregnancy advances from 1 st to third trimester, your skin changes from oily to dry skin. Use skin lotion or moisturizer.

My hair is falling out!
Because of hormonal changes, hair on your head may fall out. There is no need to worry- This is temporary and will only last until your menstrual period returns. Eat well balanced diet containing green vegetables or seaweeds.

Food cravings
Craving occurs especially during first trimester. It is normal provided you are having healthy low calorie foods. If you experience craving for clay, dirt etc., then consult your doctor.

My breast aches!
Expectant mothers breast grow larger to meet their baby needs. Some women even experience a bit of leakage at full term. Increase your bra size and wear a more supportive bra.

I am getting so stressed!!!
Tips to manage stress>
- Eat a healthy, well balanced diet
- Get plenty of sleep
- Exercise regularly, yoga or meditation
- Talk regularly with your partner
- Reduce your workload

Backache : 5 easy back ache busters
- Deep heat : Ask your partner to rub your back or indulge in a pregnancy massage. Simply apply the heat pack for approximately 15-20 minutes to your sore back as often as every 3-4 hours
-
Posture pointers:
- Always stand up tall and straight with your shoulders back – as if trying to get your head to touch the ceiling
- When sitting make sure your back is supported by a small pillow in the curve of your spine to encourage you to sit up straight
- Don’t wear high heels!
- Sleep easy: y: Try lying on your side to take stress off your lower back. Placing a pillow between your legs to support the weight of your top leg and decrease low back strain
- A daily walk of between 20 and 30 minutes can do wonders
- Back care: Never, ever, bend with your legs straight and always squat or kneel to pick up objects off the floor, keeping your back straight
MYTH SMASHER’S
FOR MOTHERS –TO-BE
Pregnant women should not have sex
#1 MYTH SMASHER
Sex during pregnancy does not hurt the baby but watch out for sexually transmitted diseases. However in women who have threat of miscarriage or unexplained vaginal bleeding, low lying placenta, sexual intercourse should be avoided.

Pregnant women should avoid travel
#2 MYTH SMASHER
Travelling short distance is no harm, but travel comfortably. Wear your seat belt while driving. Avoid long distance travelling. Avoid travelling by two & three wheelers. Do not drive.

Pregnant women should avoid exercise
#3 MYTH SMASHER
Exercise improves muscle tone, prevents low back pain, leg cramping, reduces constipation, improves mood. Exercises such as walking, swimming, cycling on stationary bike can be done. Aim for at least 30 min. of daily moderate intensity activity. Eat a light snack 30-60min. prior to workout, drink water. Stop exercise if shortness of breath, vaginal bleeding or loss of fluid from vagina, uterine contractions, chest, leg, joint or stomach pain.

Once a woman is pregnant, she needs to eat for two
#4 MYTH SMASHER
A pregnant woman needs to add 400 to 500 Kilocals. to her diet and consciously consume a balanced diet with fruits and greens. She needs two fruits a day, plenty of vegetables, a serving of tubers and shoots, milk and at least 10 to 12 glasses of water a day.
http://www.deccanherald.com/content/255491/pregnancy-myths-busted.html
Tips to be the perfect birth partner
FOR FATHERS-TO-BE

Be aware of what she wants
Talk to your wife beforehand about what she wants and doesn't want during labour. You're the one who may need to take charge and let the gynecologist know.

Look after yourself!
The mum-to-be is the center of attention, but you'll probably be spending the night at the hospital too, so don't forget to pack some things for yourself. Pack a clean T-shirt, too. Being able to change will help you feel fresher if you're up all night. Also remember to take something to eat and drink - you could be at the hospital for a while.

Know what to expect
Labour is not the right time to be flipping through a pregnancy and birth manual, so bone up on your reading beforehand. Going to antenatal classes will help. You'll get solid, basic information about what labour and birth entails, as well as a sense of how other dads- to-be are planning the event.

Be flexible
Labour strategies that work for some women, may not work for your wife. A labour partner's job is to discern what works, and be prepared to drop what doesn't.
Well before your baby's due date, you and your wife should take time to discuss her expectations and options. Later, you will be able to take the initiative while keeping her wishes in mind.

Be ready to do some hard work yourself!
Giving birth is often a long, hard job. At some point during the hours of labour, you and your wife will discover something she can focus on during contractions. It could be a breathing pattern, a spot on the ceiling, or even a soft baby toy you've brought with you. Your job is to help your wife find this distraction, and then bring her back to it whenever she starts to think she won't make it. Your wife will be relying on you to keep her concentration levels up.

Be prepared for surprises
Neither you nor your wife knows what labour will be like, or what will help your wife.
Be a one-person support team
Though there will be lots of experienced people around to help you, you will be your wife's most important support. Do whatever she needs, from running to the cafeteria for a cup of juice to getting her another drink or talking things through with your doctor.

Know your limits
There's a lot going on in the birth room. Be aware of what you are willing to do during the process, and what you want to leave to the professionals.

Be prepared to take charge
Only you and your wife know what you both want, but she may not be in the best condition to make hard decisions. Be ready to step in with some decisive action if the situation calls for it.

Be prepared to wait
Unlike what you see in films and on television, most women are in labour for hours before they even go to the hospital. Many couples find it more comfortable to spend the early stages of labour at home. Besides, many maternity units prefer you wait until your contractions are regular and close together before booking into the hospital.
Postnatal Care
First feed & the first few hours after birth
Your baby should get her first feed of breastmilk within the first hour of birth

The first milk, your body produces is known as colostrum. It is packed with antibodies that will help your baby fight infections and viruses in the coming days
It is also rich in protein and it has a laxative effect that helps your baby pass her first bowel movement
Breastfeeding techniques & tips
Techniques
Lying down
This position is a great way to rest and relax while your baby feeds. Lie down, with your body and your baby's body parallel. Snuggle up to your baby and bring her to your breast.

Across your lap (opposite arm)
Make yourself comfy in a chair or on the sofa. Put a pillow or cushion on your lap to support your baby. This will make feeding easier on your arms. Once your baby is comfy on the pillow, support her head with the opposite arm to the breast you are feeding from. Gently bring your baby's head to your breast.

Laid-back breastfeeding
Sit in a semi-reclined position. Lie your baby across your stomach so that her head reaches your breast. This position might work for you if you find sitting up and feeding painful for your back.

Koala hold
Place your baby on your lap in an upright position and hold him to your breast while supporting her well.

Twin positions
Make yourself comfortable, and get a large pillow or cushion to put on your lap. This will help you to support both of your babies. If possible, have someone nearby who can pass you your babies.
Try putting one baby under each arm, with their heads near your breasts. You can use the same arm as your breast to support each baby.

Under your arm
If your baby is a kicker, this may be the position for you. Place your baby so that her body is underneath one of your arms, with her head near your breast. Support her head with the same arm as your breast.
First bath for your baby
- Start with only a few inches of warm water. Your baby’s bath water should be between 32 and 37 degrees Celsius. After filling the basin or tub, be sure to swirl the water with your hands so there are no hot spots.
- Before you put your baby in the bath water, test the water’s temperature on the inside of your wrist to make sure it is not too hot.
- Using one arm to gently support your baby's back, head and neck, gently place her in the baby bath. Continue to support her using one arm while bathing her with the other.
- Gently wipe around your baby's mouth, nose and whole face, working from the middle outward. Wipe the creases in her neck and don't forget behind her ears!
- You can use a gentle cleanser formulated for babies. If your baby has more hair, you might try a gentle shampoo. Don’t be afraid to gently wash the soft spots (called fontanels) on your baby's head.
NOTE: Be sure that your home’s hot water heater is set no higher than 48 degrees Celsius to help protect against accidental scalding.
- Wash the diaper area last. For a baby girl, cleanse the genital area washing from front to back. For boys, gently wash the penis and genital area, also washing from front to back, and dry thoroughly. For an uncircumcised boy, avoid pulling back the foreskin.
- Let your baby take a few moments in the bath to enjoy the warm water. Pour cupfuls of water over her body to keep her warm. Be mindful of running water directly from the tap as water temperature can sometimes change suddenly.
- Wrap both hands around your baby's chest under her arms, support her head, and lift her out of the bath and quickly wrap her in a towel.
- Dry your baby well in all the creases, as excessive moisture could lead to skin irritation. Pat her skin dry to avoid skin damage.
- Before dressing your baby, apply a gentle baby powder and a gentle baby moisturizer, such as hypoallergenic which is clinically proven to be gentle and mild.
Care for your baby
Massage

Resting hands
Begin with a resting hand technique. It can also be used when your baby needs a break during the massage. This is a good way for your baby to feel secure and enjoy touch.
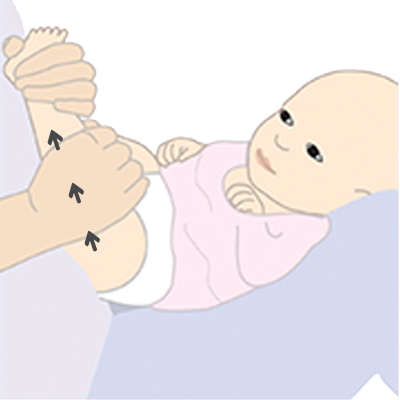
Legs
Put oil on your hands and start with her legs because it is an area which is usually accepted by babies. Downward strokes are more relaxing.

Legs – milking
With one hand, gently hold your baby’s ankle. Place your other hand at the top of your baby’s thigh, molding it around the leg, then slide it to the ankle. Repeat with firm yet gentle rhythmic strokes, one hand after the other.

Feet
Watch your baby’s reactions in case of sensitivity. Gently squeeze and roll each toe between your thumb and index finger. Using alternate thumbs, stroke the top of the foot from the toes to the ankle. Repeat several times.

Tummy
When baby’s umbilical cord is healed, gentle massage on the tummy can help with digestion and tummy troubles. Make gentle paddling strokes, with one hand following the other.

Back
Skin-to-skin contact can enhance the bonding experience between baby, mum and dad. Holding the baby close to your chest, massage your baby’s back beginning at the neck, swooping down to their bottom.
Bathing
- Make sure everything you need - Towel, clothes, diaper, baby wash is within reach before you start. NEVER leave the baby unattended in water, not even for a moment.
- Fill your tub (with a non-slip mat at bottom) with a few centimetres of warm water. The temperature of the bathing water should be kept close to the body temperature (around 37oC). Swirl the water gently to ensure there are no hot spots, and test the temperature with the inside of your wrist before you place baby in the water.
- Support the baby with one hand, while you wash with the other. Wet the washcloth with warm water, and wash the baby’s eye area from the inside corner to the outside corner. Then add a small amount of cleanser, and continue to clean from top to bottom. To clean the scalp, use a wet washcloth and a tiny amount of baby shampoo. Rinse the washcloth and use it to wipe off the shampoo. Be sure to always wash the diaper area from front to back.
- Rinse the baby with small cupfuls of water. Use water from the tub, not directly from the faucet, as water temperatures can vary unexpectedly.
- Lift the baby gently out of the tub and dry with a soft towel.


Umbilical Cord Care
- Before cleaning your baby's umbilical cord, you can put her shirt and diaper on to keep her warm.
- Remember to avoid covering the cord with the diaper, because the cord area should be kept dry and clean at all times.
- Clean around and in the base of the cord with a cotton ball.
- Do not be afraid to clean the cord; the quicker the base dries, the sooner the cord will fall off
Sleep
A clinically proven BEDTIME ROUTINE can help baby fall asleep faster and stay asleep longer in a simple 3-step before bed routine to help babies sleep better in just one week.



Warm Bath
Bath time is the perfect way to start your baby’s pre-bed routine. Use a wash with an enjoyable and familiar scent to help your baby sleep better. In studies, babies bathed with a fragranced bath product (compared to those who weren’t) spent nearly 25% less time crying before sleep.

Baby Massage
A soothing massage is a wonderful way to make your baby feel secure, loved and ready for sleep. Research has shown that routine touch and massage improves sleep quality and quantity when part of a bedtime routine. Massage can also help you recognise and respond to your baby's body language and it also makes your little one feel safe and secure.

Quiet Time
Soft lullabies and dim lighting helps baby settle. You can help your baby wind down further by reading or singing softly. It's best to avoid active play at this time, so your baby goes to bed sleepy but still awake. This will help her learn how to self-soothe and get back to sleep on her own if she wakes up during the night.

Nappy care
50 to 60% of all babies will suffer from diaper rash at some time. Diaper rash can lead to an increased frequency of crying, changes in eating habits and sleep patterns, agitated and restless behavior and sometime less urination and/or defecation to avoid pain. Careful care when changing your baby’s diaper can help prevent diaper rash.
Diaper Rash Management
Follow the 3Cs

Change
Keep baby’s skin dry and clean by changing dirty diapers as soon as possible.

Clean
Use mild baby wipes which also contains moisturizer like Johnson’s® Baby Wipes to gently cleanse and moisturize the delicate skin.

Cover
Apply Diaper Rash Cream to entire diaper area with each diaper change.
How to prevent diaper rash
- Be careful not to apply your baby’s diaper too tightly.
- Let your baby go without her diaper as much as possible.
- Apply Johnson’s® Baby Diaper Rash Cream with each diaper change.
- Change your baby’s diaper frequently.
- Choose the right size diaper.
Few quick tips on nappy care
- Keep your baby clean and dry by changing the diaper frequently.
- Clean your baby’s diaper area well at each diaper change. Remember to pat her skin dry, don’t rub.
- Don’t put on the diaper too tight, as it allows better air circulation and speeds healing. You could even let your baby sleep with a bare bottom.
- If the problem still persists, you should immediately contact a doctor.
3-STEP BABY SKIN CARE ROUTINE
Moisturize and protect baby’s skin with a 3-step baby skin care routine

Clean
Bathe or cleanse the skin to remove impurities with a cleanser of documented mildness

Dry
Maintain hydration and protect the skin barrier by using a moisturizing lotion

Apply
Apply Diaper Rash Cream to entire diaper area with each diaper change.
Postnatal depression
The "baby blues"
Postnatal depression is a type of depression that many mothers experience after having a baby

Persistent feeling of sadness and low mood

Trouble sleeping at nigh

Problems concentrating and making decisions

lack of enjoyment and loss of interest
Postnatal massage
The postnatal massage is a full body massage that is given to a mum every day for up to 40 days after birth
- To ease sore spots and relax muscle tension
- Increase the flow of blood and oxygen to mother’s muscles, getting rid of the toxins
- Speed up recovery from a caesarean section if you've had one

Tips for New dad
Hold your nerve
This is the time to stay calm and remind your wife what a great job she has done so far

Pamper her
Run your wife a relaxing bath, massage her shoulders, arrange for favorite meals, and bring her snacks as well as drinks while she breastfeeds.

Talk and listen
listen: You and your wife really can't do enough of this. Give your baby and wife equal amounts of praise, and be honest about how becoming a parent has made you feel. In return, you need to listen to her, and understand that while she may feel weepy and ecstatic all at the same time, all she needs from you is love and support.
This module on antenatal care was developed in the supervision of the following expert gynecologist
Dr. Alka Kriplani
Imm. Past President, FOGSI-2016
Dr. Garima Kachhawa
Jt . Secretary, FOGSI 2016
Dr. Archana Verma
Chairperson Public awareness committee, FOGSI
Dr. Aparna Sharma
Co-convenor FOGSI foetal medicine & genetics committee
PREGNANCY PLANNER
This module on antenatal care was developed in the supervision of the following expert gynecologist
Dr. Archana Verma
Chairperson
Public awareness committee, FOGSI
Dr. Alka Kriplani
Imm. Past President, FOGSI-2016
Dr. Archana Verma
Co-convenor
FOGSI foetal medicine & genetics committee
Dr. Garima Kachhawa
Jt . Secretary
- The content is licensed by
- (The Federation of Obstetric and Gynecological Societies of India)
Disclaimer: This information of a general nature and is designed for educational purposes only. If you have any concerns about your own health or the health of your child, you should always consult with a doctor or other healthcare professional.

PLANNING ANTENATAL CLASSES

Content of the sessions
SESSION 1: (0-12 weeks)
- Changes in the body and how baby grows inside you
- What tests to be done for you and your baby
- How to deal with discomforts and keep you and baby health
- Exercises
- Lifestyle advice
- Easy ways to eat healthy
- Understanding danger signs
SESSION 2: (12-28 weeks)
- What tests to be done for you and your baby
- Easy ways to eat healthy
- Understanding danger signs
Session 3 (30-36 weeks)
- Understanding danger signs
- Prepare for labor and delivery
- After The baby is born how will you feel
- Caring for the baby
- Infant feeding
Average normal pregnancy lasts for
283 days, or 40 weeks
Conventionally, it has been divided into 3 trimesters
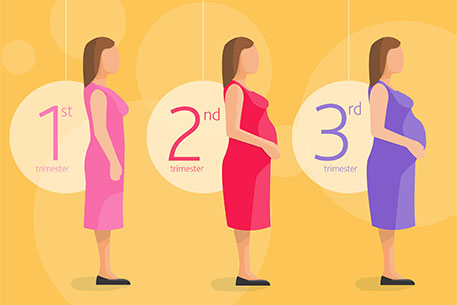
WEEK 0-13
FIRST TRIMESTER:
- Baby develops from just a few cells, the size of a pin head to about 7cms in this trimester
- Fetus most susceptible to effects of medicine.
- You may experience cravings, morning sickness, fatigueand frequent urination

WEEK 14-26
SECOND TRIMESTER:
- Troublesome symptoms of first trimester fading
- Stretch marks start appearing on abdomen
- Mother can feel the baby movements at 16-18 weeks
- By 26 weeks, eyes and ears of baby begin functioning, baby can open and clench hands
- Go for regular health check-ups
- Eat nutritious food and exercise
- Join swimming and yoga classes
WEEK 27-40
THIRD TRIMESTER:
- You may experience swelling of feet, constipation, backache
3 rd TRIMESTER CHECK LIST
- Take proper sleep
- Do some stretching exercises
- Eat healthy
- Be prepared for breastfeeding
- Always be aware about baby’s movement
- Always keep a hospital number handy
THINGS TO EXPECT AND TIPS TO HANDLE THEM
- First clue that you might be pregnant
- Consult your doctor
- Get urine pregnancy test done
- Eat foods rich in iron and protein
- Take daytime naps when you can
- Regular exercise
- Take rest
- Eat more fresh fruit and vegetables
- Drink 8-10 glasses of water a day
- Eat foods with lots of fibre
- Exercise regularly
- Rest with your legs up
- Lie on your left side while sleeping
- Take breaks from sitting or standing and take a short walk
- Exercise
- Drink plenty of fluids
- Sip ginger or grate it fresh in tea or try ginger candy
- Eat small frequent meals
- Opt for cold dishes, which gives off fewer aromas
- Non greasy meals with little odor such as fresh fruits, raw almonds, whole grain toast before getting out of bed.
- Limited caffeinated foods and beverages
- Eat small, frequent meals
- Avoid spicy or greasy foods
- Try drinking milk before eating
- Don’t lie down right after eating
- Elevate the head of bed 6-8 inches when lying down
- Don’t overeat
- Avoid alcohol, chocolate, coffee and tea
- Increase your bra size and wear a more supportive bra
- Gently stretch the calf of your leg by pointing your toes upward, toward your knee
- Need to empty bladder often as a growing baby puts pressure on bladder
- Can’t be helped and is normal
- Eat bananas, white rice, oatmeal and refined white bread

MYTH SMASHER
PREGNANT WOMEN SHOULD AVOID EXERCISE
- Exercise improves muscle tone, prevents low back pain, decreases chances of varicose veins, leg cramping, reduces constipation, improves mood
- Exercises which can be done: walking, swimming, cycling on stationary bike
- Aim for at least 30 min. of daily moderate intensity activity
- Avoid lifting very heavy weights
- Do not overexert yourself or exercise upto exhaustion
- Eat a light snack 30-60 min. prior to workout, drink & water
- Do not exercise if you have hypertension, ruptured membranes, bleeding per vaginum, preterm labour, incompetent cervix or other medical conditions
- Stop exercise if shortness of breath, vaginal bleeding or loss of fluid from vagina, uterine contractions, chest, leg, joint or stomach pain
PREGNANT WOMEN SHOULD AVOID TRAVEL
- Travelling short distance is no harm, but travel comfortably
- Wear your seat belt while driving
- Avoid long distance travelling
- Avoid travelling by two & three wheelers
- Do not drive
- Should consult your doctor before air travel
PREGNANT WOMEN SHOULD NOT HAVE SEX
- Sex during pregnancy does not hurt the baby but watch out for sexually transmitted diseases. However in women who have threat of miscarriage or unexplained vaginal bleeding, low lying placenta, sexual intercourse should be avoided.
BALANCED DIET DURING PREGNANCY
EAT A VARIETY OF FOOD TO GET ALL THE NUTRIENTS
- You need 300 extra calories each day
- 3-4 glasses of milk
- Dairy products: 4 servings
- Fruits : 2-4 servings
- Bread and grains: 6-11 servings
- Protein products : 3 servings
- At least 6-8 glasses of liquids
- Sweets, spices, fried or fast foods, commercially baked foods in moderate quantity only
HIGH FIBRE DIET:
Whole grain breads, cereals, pasta, rice, fruits, vegetables
DAIRY PRODUCTS:
To get 1000-1300mg calcium in daily diet
ONE SOURCE OF VITAMIN C EVERY DAY
Oranges, grapefruits, strawberries, papaya, broccoli, tomatoes
ONE GOOD SOURCE OF FOLIC ACID EVERY DAY
Dark green leafy vegetables, legumes, beans, chickpeas, blackbeans
AT LEAST ONE SOURCE OF VITAMIN A EVERY OTHER DAY
Carrots, pumpkins, sweet potatoes, spinach, apricots
WEIGHT GAIN DURING PREGNANCY
- About 11-14 Kgs is required
- If you are overweight when you get pregnant, you may need to gain only 7-11 Kgs
KEEP IRON LEVELS UP
- Take iron supplements prescribed by your doctor
- Iron pills are not to be taken on an empty stomach
- Don’t drink milk with an iron rich meal
- Don’t take tea or coffee with meals or iron supplements
- Cooking in iron vessels may increase iron content of food. Do this no more than 2-3 times a week
- Add few drops of lime to dal, curries, sprouts or other iron rich food
- You can also drink lemonade or orange juice with your meals
- Sources of iron: green leafy vegetables, cauliflower, fenugreek, mint, lentils, beans, chicken, fish, egg, dried fruits such as apricots, raisins
FOODS TO AVOID
- Avoid raw and uncooked food
- Unpasteurised milk or cheese
- Fish high in mercury content
- Excessive intake of caffeine
- Alcohol intake
- Artificial sweeteners
WATCH YOUR POSTURE

STANDING
While standing, do not exaggerate the hollow of your back. Stand with feet apart and hold your head up

SITTING
While sitting, sit so that the whole length of your thighs are supported by the seat. If needed, a cushion can be placed between the back rest and your back. Take support of the back of the chair and sit straight

SLEEP
The best sleep position during pregnancy is sleeping on your side. Even better is to sleep on your left side

GETTING UP FROM A LYING DOWN POSITION
The best sleep position during pregnancy is sleeping on your side. Even better is to sleep on your left side

LIFTING
While lifting and carrying, do not bend your waist. Keep your back straight and bend your knees and hips
PREGNANCY FITNESS
PELVIC FLOOR EXERCISES
Imagine trying to stop passing wind and hold your flow of urine at the same time. The feeling is of squeeze and lift pulling up and in around your front and back passages
Hold the squeeze for upto 10 seconds
Do 3 or 4 sets, three times a day

DOS IN PREGNANCY
- Regular monthly check-up is necessary
- Eat balanced diet
- Take small, frequent meals if required
- Have plenty of water
- Always remain in a good, cheerful and relaxed mood and also maintain a pleasant atmosphere with good ventilation and airy rooms
- A minimum of half an hour walk at fairly brisk pace is a good exercise
- Sleep at least 8 hours in night & 1-2 hours in day time
- While picking up things from the floor, sit down & then lift
- Wear your seat belt while driving
DONT'S IN PREGNANCY
- Don’t take any medicine without doctors advice
- Don’t overeat; avoid junk food, fried or oily food
- Don’t smoke
- Don’t wear high heeled shoes
- Don’t take unnecessary tension & avoid stress
- Don’t take too much rest & avoid oversleeping
- Don’t bend down with straight legs
- Avoid travelling by two or three wheelers
- Do not drive
- Don’t carry heavy weight
- Don’t wake up suddenly with a jerk
- Avoid long distance travelling
ANTENATAL SCHEDULE

FIRST ANC VISIT:
As early as possible, preferably in the first trimester
- Folic acid
- Weight and BP record
- Blood Group and RhD status
- creening for anaemia (Hb), syphilis(VDRL), hepatitis B virus (HbSAg), HIV
- Blood Sugar (fasting and PP)
Second Teimester (Week 11 - 22)
To make out the chromosomal anomalies
As early as possible, preferably in the first trimester
- Dual screen at 11-13 wks
- Triple screen 16 wks
- Level II screening at 18-20 wks
Quadruple screening test alpha fetoprotein, human chorionic gonadotropin, unconjugated estriol, inhibin A (15-22 weeks)
SECOND VISIT:
- Iron, calcium
- Blood pressure and test urine for proteinuria
- Screening for gestational Diabetes if possible
- Anti-D to rhesus negative women
- TT immunisation (2 doses
THIRD VISIT:
- Folic acid, iron, calcium
- Blood pressure and test urine for proteinuria
- Second screening for anemia
- Ultrasound scan for fetal growth, placenta localisation, liqour
FOURTH VISIT:
- Folic acid, iron, calcium
- Blood pressure and test urine for proteinuria
FAQs
As your womb grows larger, ligaments stretch and you feel this in your groin area. By sleeping on your side with the leg that hurts on the bottom, the ligaments will relax and pain decreases. Take enough calcium
As your pregnancy advances from first to third trimester, your skin changes from oily to dry skin. Use skin lotion or moisturiser
Because of hormonal changes, hair on your head may fall out. There is no need to worry- this is temporary and will only last until your menstrual period returns. Eat well balanced diet containing green vegetables or seaweeds
Expectant mother’s breasts grow larger to meet their baby’s needs. Some women even experience a bit of leakage at full term. Increase your bra size and wear a more supportive bra.
Craving occurs especially during first trimester. It is normal provided you are having healthy low calorie foods. If you experience craving for clay, dirt etc., then consult your doctor
- Eat a healthy, well balanced diet
- Get plenty of sleep
- Exercise regularly with yoga or meditation
- Talk regularly with your partner
- Reduce your workload

Ask your partner to rub your back or indulge in a pregnancy massage. Simply apply the heat pack for approximately 15-20 minutes to your sore back as often as every 3-4 hours
- Always stand up tall and straight with your shoulders back – as if trying to get your head to touch the ceiling
- When sitting make sure your back is supported by a small pillow in the curve of your spine to encourage you to sit up straight.
- Don’t wear high heels!
Try lying on your side to take the stress off your lower back. Place a pillow between your legs to support the weight of your top leg and decrease low back strain
Never, ever, bend with your legs straight and always squat or kneel to pick up objects off the floor, keeping your back straight
- Any leaking or bleeding per vaginum
- Decreased baby movements
- Pain or cramps in your abdomen
- Sudden or extreme swelling of your face or fingers
- Severe headache
- Blurring of vision
- Less urine or burning when you void
- Chills or fever
- Repeated vomiting